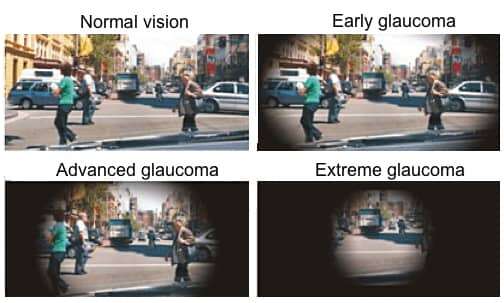
Glaucoma is a chronic, progressive eye disease that damages the optic nerve, which connects the eye to the brain. This damage is often caused by abnormally high pressure in the eye. Glaucoma is the second leading cause of blindness worldwide, affecting approximately 80 million people.
What makes glaucoma particularly dangerous is its silent progression in many cases. About 50% of people with glaucoma don’t know they have it because the early stages often produce no symptoms. By the time vision problems become noticeable, permanent damage may have already occurred.
When I was diagnosed with acute angle-closure glaucoma a few years ago, it came as a shock despite my lifelong history with vision problems. Unlike my astigmatism, which was manageable with glasses, glaucoma presented a much more serious threat to my sight.
There are several types of glaucoma, each with different characteristics:
Open-Angle Glaucoma
The most common form, accounting for about 90% of all cases. It develops slowly as the drainage canals become clogged over time, increasing eye pressure. Most people have no symptoms until vision loss begins.
Angle-Closure Glaucoma
This occurs when the iris bulges forward, narrowing or blocking the drainage angle between the cornea and iris. When this drainage angle becomes completely blocked, eye pressure rises quickly, resulting in an acute attack.
Congestive Glaucoma
This is what my ophthalmologist diagnosed me with. During an acute attack, I experience severe throbbing eye pain, redness, headaches, and nausea. The world appears cloudy, as though I’m seeing everything through a thick fog, and lights have halos around them. These episodes come on suddenly and are terrifying experiences.
Normal-Tension Glaucoma
In this form, optic nerve damage occurs despite normal eye pressure levels. The cause is not fully understood, but may be related to poor blood flow to the optic nerve.
Secondary Glaucoma
This type results from other medical conditions, injuries, or medications that increase eye pressure.
This morning, I couldn’t see my daughter’s face clearly while helping her get dressed for school. The buttons on her uniform blurred together, and I had to feel my way through each one. These daily challenges remind me of what’s at stake with this condition.
My medication routine is exhausting and dictates my entire day:
Azopt: Three times daily (6am, 12pm, 6pm). Each bottle costs around GHS 250 monthly and only lasts about two weeks. It gives me cloudy vision immediately after application, worsening my already blurry vision for at least an hour. This means my vision is compromised when I’m traveling to work, during work, and on my way home.
Timolol: Twice daily. I must wait 5 minutes after Azopt before applying this.
Pilocarpine: Three times daily. These drops are often scarce in Ghana where I live, and when I do find them, they make it even harder to recognize people’s faces.
Natural tears: Four times daily. I need to wait another 5 minutes after Timolol before using these.
Oral medication: I sometimes take tablets as well as part of my treatment.
This intricate regimen requires me to space out drops 5 minutes apart each time. Some days, I become overwhelmed by the routine and think “what can come, can come” because I’m just so tired of the constant vigilance. Other times, I desperately want relief from the constant congestion in my eyes.
Certain factors increase the risk of developing glaucoma:
– Family history (having a parent or sibling with glaucoma)
– Age over 60 (or over 40 for African Americans)
– African, Asian, or Hispanic descent
– High internal eye pressure
– Certain medical conditions like diabetes, heart disease, or high blood pressure
– Previous eye injury or surgery
– Extreme nearsightedness or farsightedness
– Long-term use of corticosteroid medications
Glaucoma runs in my family. My father is completely blind in one eye and has about 60% vision loss in his other eye from the same type of glaucoma I have. This family connection makes me especially vigilant about my children’s eye health, both of whom have already been diagnosed with astigmatism at young ages.
While there is no cure for glaucoma, several treatments can help manage the condition and slow its progression:
Eye drops are typically the first line of treatment. They work by either reducing fluid production in the eye or improving drainage. Some common types include:
– Prostaglandin analogs
– Beta blockers (like my Timolol)
– Alpha-adrenergic agonists
– Carbonic anhydrase inhibitors (like my Azopt)
– Rho kinase inhibitors
– Miotic or cholinergic agents (like my pilocarpine)
Several laser procedures can help improve drainage:
– Laser trabeculoplasty (for open-angle glaucoma)
– Laser iridotomy (for angle-closure glaucoma)
– Cyclophotocoagulation (reduces fluid production)
When medication and laser treatments aren’t effective, surgical options include:
– Trabeculectomy (creates a new drainage pathway)
– Drainage implants
– Minimally invasive glaucoma surgery (MIGS)
Astigmatism is an entirely different eye condition but often coexists with other vision problems. It occurs when either the cornea (front surface of the eye) or lens has an irregular curve, causing blurred vision at all distances.
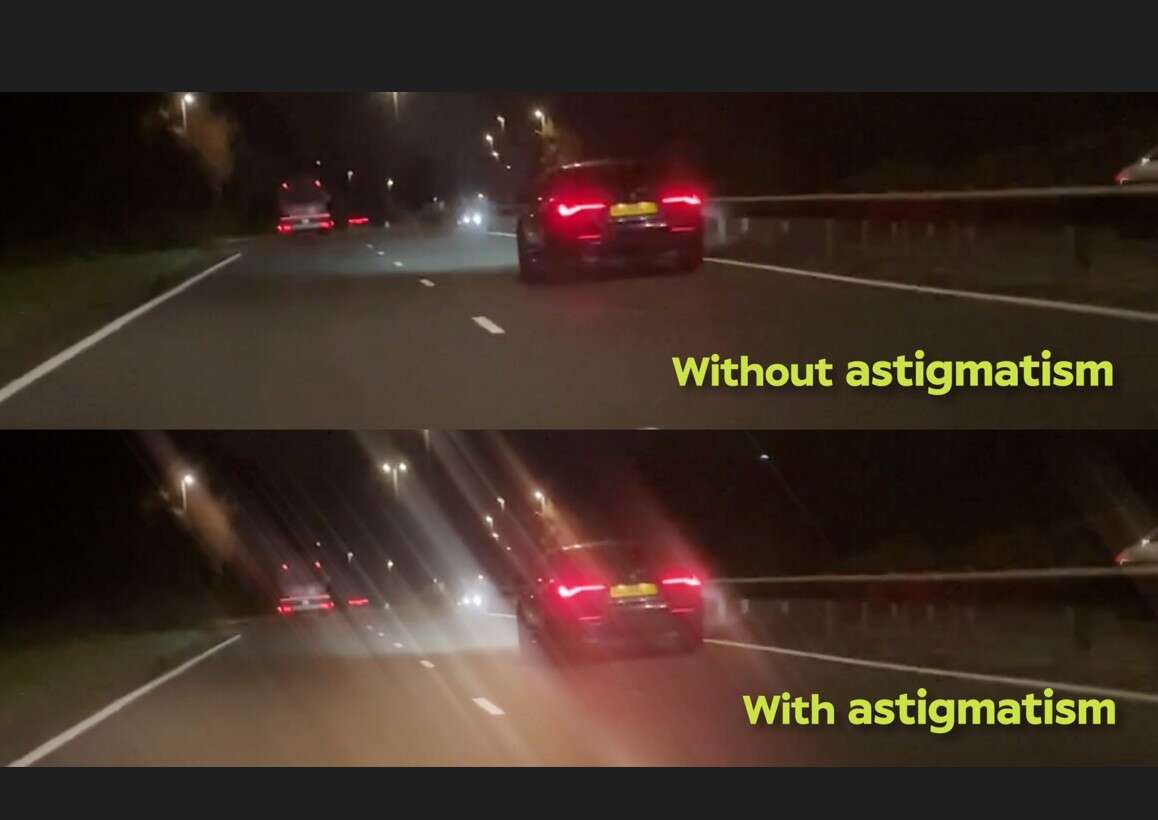
Unlike glaucoma, astigmatism is a refractive error, not a disease. It’s extremely common, with most people having some degree of astigmatism.
– Blurred or distorted vision at all distances
– Eyestrain
– Headaches
– Squinting to see clearly
– Poor night vision
I’ve had astigmatism since childhood. While it’s manageable with corrective lenses, dealing with both astigmatism and glaucoma creates additional challenges. When I read too much, my eyes hurt, and I get headaches and eye pain.
Astigmatism is typically corrected with:
– Eyeglasses
– Contact lenses (toric lenses)
– Refractive surgery (LASIK, PRK, or SMILE)
Managing chronic eye conditions involves both medical treatment and lifestyle adaptations.
Working in public relations means I spend most of my day reading and writing. These tasks have become increasingly difficult as the letters on my keyboard seem to dance and shift. Sometimes I see ‘e’ as ‘a’. Reading requires multiple attempts to understand the text.
I’ve developed strategies to maintain my quality of life:
– Using larger fonts on devices
– Taking regular breaks when reading
– Working in appropriate lighting conditions
– Organizing spaces to locate items easily
– Using voice recognition software when necessary
The financial burden of managing glaucoma is significant. In Ghana, medications are expensive and often in short supply. Azopt alone costs around GHS 250 per bottle, and I need it monthly, with each bottle only lasting about two weeks. With multiple medications required daily, the costs add up quickly, adding financial stress to an already challenging condition.
Regular comprehensive eye exams are crucial for detecting glaucoma before significant damage occurs. The frequency depends on age and risk factors:
– Under 40: Every 2-4 years
– 40-54: Every 1-3 years
– 55-64: Every 1-2 years
– 65 and older: Every 6-12 months
People with high risk factors should be checked more frequently as advised by their eye care professional.
One of the hardest parts of living with glaucoma in Ghana is the lack of support systems. There are no functioning support groups where I can talk about my fears with others who understand what I’m going through. Doctors provide medical treatment, but they can’t offer the perspective of someone living with the condition.
This is why I’m writing – because nobody truly understands what it means to be living with a degenerative optic nerve condition. I know my friends and family mean well, and I appreciate their concerns, but sometimes I just want to be quiet and not talk about it. The mental strain of knowing my vision is slowly deteriorating is sometimes as overwhelming as the physical symptoms themselves.
Research into new treatments for glaucoma continues to advance. Scientists are exploring:
– Neuroprotection strategies to directly protect the optic nerve
– Gene therapy
– Stem cell approaches
– New drug delivery methods that require less frequent administration
– More effective surgical techniques
My greatest fear is waking up one day and not being able to see my children. As someone who has always loved reading and writing – from the novels I devoured as a young girl to my current career writing releases, Op-eds, articles, reports, PR plans, Event budgets – the prospect of losing my vision affects not only my daily activities but my very identity.
Glaucoma remains a serious threat to vision worldwide, but early detection and consistent treatment can help preserve sight for most patients. Regular eye examinations are essential, especially for those with risk factors.
The reality of living with glaucoma goes beyond the clinical aspects. It’s a daily struggle with medication routines, side effects, expenses, and the emotional weight of a progressive condition. Some days are better than others, and maintaining hope while being realistic about my condition is a delicate balance.